12/10—Vaccine deployment plans in the EU/UK
Overview of COVID-19 vaccination strategies and vaccine deployment plans in the EU/EEA and the UK
This document outlines the initial developments in EU/EEA member states and the UK regarding vaccine deployment plans and national vaccination strategies for COVID-19 vaccines, including interim considerations for priority groups, evidence to be considered for the prioritisation of target groups, logistical considerations and monitoring systems for post-marketing surveillance (e.g. vaccine coverage, safety, effectiveness and acceptance).
SARS-CoV-2 infection and transmission in educational settings: a prospective, cross-sectional analysis of infection clusters and outbreaks in England
A median of 38 000 early years settings (IQR 35 500–41 500), 15 600 primary schools (13 450–17 300), and 4000 secondary schools (3700–4200) were open each day, with a median daily attendance of 928 000 students (630 000–1 230 000) overall. There were 113 single cases of SARS-CoV-2 infection, nine coprimary cases, and 55 outbreaks. The risk of an outbreak increased by 72% (95% CI 28–130) for every five cases per 100 000 population increase in community incidence (p<0·0001). Staff had higher incidence than students (27 cases [95% CI 23–32] per 100 000 per day among staff compared with 18 cases [14–24] in early years students, 6·0 cases [4·3–8·2] in primary schools students, and 6·8 cases [2·7–14] in secondary school students]), and most cases linked to outbreaks were in staff members (154 [73%] staff vs 56 [27%] children of 210 total cases). Probable direction of transmission was staff to staff in 26 outbreaks, staff to student in eight outbreaks, student to staff in 16 outbreaks, and student to student in five outbreaks. The median number of secondary cases in outbreaks was one (IQR 1–2) for student index cases and one (1–5) for staff index cases. SARS-CoV-2 infections and outbreaks were uncommon in educational settings during the summer half-term in England. The strong association with regional COVID-19 incidence emphasises the importance of controlling community transmission to protect educational settings. Interventions should focus on reducing transmission in and among staff.
Detecting COVID-19 infection hotspots in England using large-scale self-reported data from a mobile application: a prospective, observational study
In this prospective, observational study, we did modelling using longitudinal, self-reported data from users of the COVID Symptom Study app in England between March 24, and Sept 29, 2020. A total of 2 873 726 users living in England signed up to use the app, of whom 2 842 732 (98·9%) provided valid age information and daily assessments. These users provided a total of 120 192 306 daily reports of their symptoms, and recorded the results of 169 682 invited swab tests. On Sept 28, 2020, we estimated an incidence of 15 841 (95% CI 14 023–17 885) daily cases, a prevalence of 0·53% (0·45–0·60), and R(t) of 1·17 (1·15–1·19) in England. On a geographically granular level, on Sept 28, 2020, we detected 15 (75%) of the 20 regions with highest incidence according to government test data. Our method could help to detect rapid case increases in regions where government testing provision is lower.
Does respiratory co-infection facilitate dispersal of SARS-CoV-2? investigation of a super-spreading event in an open-space office
[Via Public Health England.] Authors describe a super-spreading event within a team working in an openspace office and investigate factors potentially having facilitated SARS-CoV-2 transmission. Of 13 team members, 11 fell ill with COVID-19. Sequence of events and full genome sequence data suggest one person as index case, directly infecting 67 to 83% of the teammates. The index case and a further individual were diagnosed with an adenovirus serotype 4 co-infection. Several environmental and behavioural factors identified that probably facilitated the transmission. Relevance of the adenovirus co-infection remains unclear and merits further investigation.
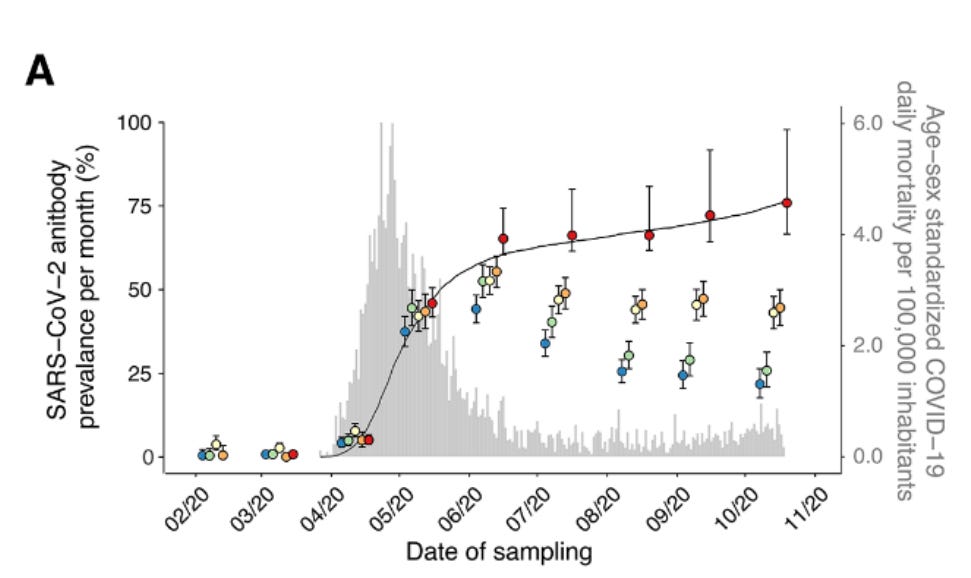
Three-quarters attack rate of SARS-CoV-2 in the Brazilian Amazon during a largely unmitigated epidemic
SARS-CoV-2 spread rapidly in the Brazilian Amazon and the attack rate there is an estimate of the final size of a largely unmitigated epidemic. We use a convenience sample of blood donors to show that by June, one month after the epidemic peak in Manaus, capital of Amazonas state, 44% of the population had detectable IgG antibodies. Correcting for cases without a detectable antibody response and antibody waning, we estimate a 66% attack rate in June, rising to 76% in October. This is higher than in São Paulo, in southeastern Brazil, where the estimated attack rate in October is 29%. These results confirm that, when poorly controlled, COVID-19 can infect a high fraction of the population causing high mortality.
Missed an update? View past issues.