10/6—Guidance for the Prevention of the COVID-19 Epidemic in Long-Term Care Facilities
A questionnaire was sent and systematically accompanied by phone call to the 132 Long-term Care Facilities (LTCFs) of Haute-Garonne (South-West of France). 124 LTCFs participated (93.9%); 30 (24.19%) were contaminated with COVID-19. Public LTCFs (OR= 0.39 (0.20-0.73), LTCFs which organized staff compartmentalization within zones (OR= 0.19 (0.07-0.48)), and LTCF with a staff who self-assessed a higher quality implementation of the preventive measures (OR= 0.65 (0.43-0.98)) were significantly more likely to avoid contamination by the COVID-19 outbreak. Our study supports the relevance of guidance to prevent the entry of COVID-19, in particular the staff compartmentalization within zones (Rolland et al. 2020).
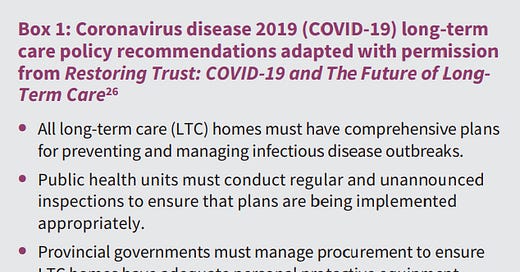
COVID-19 in long-term care homes in Ontario and British Columbia
Many more residents living in Ontario long-term care homes have died from coronavirus disease 2019 (COVID-19) than in British Columbia. Before the pandemic, the long-term care system in British Columbia exhibited a number of potential strengths relevant to pandemic preparedness compared with Ontario: there was better coordination between long-term care, public health and hospitals; greater funding of long-term care; more care hours for residents; fewer shared rooms; more nonprofit facility ownership; and more comprehensive inspections. During the first wave of the pandemic, British Columbia was faster than Ontario in responding to COVID-19, with actions to address public health support, staffing, and infection prevention and control.

Impact of meteorological conditions and air pollution on COVID-19 pandemic transmission in Italy
Our main findings highlight that temperature and humidity related variables are negatively correlated to the virus transmission, whereas air pollution (PM2.5) shows a positive correlation (at lesser degree). In other words, COVID-19 pandemic transmission prefers dry and cool environmental conditions, as well as polluted air.
The impact of temperature, population size and median age on COVID-19 (SARS-CoV-2) outbreak
This study aims to explore the association between the spread of COVID-19 and external parameters. Temperature, population size, median age, and health care facilities of 58 different countries are considered as external factors. The temperature, population size, and median age are positively associated with the spreading rate of COVID-19. There is no evidence supporting that case counts of COVID-19 could decline in countries with better health care facilities.
Meta-Analysis: COVID-19 Disease Severity Correlates with Smoking Status
We have been able to demonstrate the statistical significance in this regard of twelve series from China, France and in the US, reporting three different smoking status (current smoker, former smoker, with a smoking history) as well as disease severity (with respectively odds-ratio of 1.78 [1.08-3.10], 4.60 [3.13-7.17], 2.74 [0.63-5.89]).
Get it by email:
Missed an update? View past issues.