UK Committee opts not to recommend vaccination of 12-15 year olds
Covid-19: JCVI opts not to recommend universal vaccination of 12-15 year olds
The UK’s Joint Committee on Vaccination and Immunisation (JCVI) has not recommended that all young people aged 12-15 are given the covid-19 vaccination. Children aged 12-15 who are clinically vulnerable to covid-19 or who live with adults with an increased risk of serious illness from the virus are already eligible for a covid-19 vaccine and are being contacted by the NHS to be invited to come forward. The JCVI recommended on 3 September that this offer should be expanded to include more children aged 12-15, such as those with sickle cell disease or type 1 diabetes.
Rapid response to: Covid-19: JCVI opts not to recommend universal vaccination of 12-15 year olds
Dear Editor, […] Amidst the apparent controversy, it is helpful to pause and examine the case for COVID-19 vaccination carefully. Vaccination policy normally works on two levels: individual protection [and] societal protection. However, the benefit-risk calculations for children differ in important ways. In the elderly where COVID-19 mortality is up to 7% of infections, and others with major risk factors, vaccination against COVID-19 seems appropriate. The benefits likely outweigh risks. In children and young adults, the equation appears weighted towards risk. Does the vaccine protect others? Despite high hopes of gaining transmission-blocking ‘herd immunity’ through mass vaccination, this seems unachievable. From a public health standpoint, it makes poor sense to impose vaccine side-effects on people at minimal risk of severe COVID-19. The argument that it protects others is weak or contrary to evidence.
Rapid Response:
Re: Covid-19: JCVI opts not to recommend universal vaccination of 12-15 year olds
Dear Editor, […] As of September 3rd, 2021, ~5 million children in the United States have been tested positive for COVID-19. Only ~1% of those resulted in hospitalization (10-20 times less than in adults) and >70% of those children hospitalized had underlying comorbidities such as obesity. Case fatality rate in this group is also extremely low (0 - 0.03%; 100 times less than in elderly). In the absence of long-term safety data, there is a potential for harm - both for known side effects as well as the long-term unknown and unintended consequences for children. Besides local injection site reactions and systemic symptoms, the CDC has completed investigation of more serious side effects - myocarditis and pericarditis - now reported in over 1000 children and young adults and found a potential link; US FDA has issued a warning for the same. Proponents of covid-19 vaccine in children argue that children transmit viruses to vulnerable older adults. Data to back this argument does not exist. More so, the Covid vaccination rates for elderly in the United States (and in western countries) is relatively very high which should provide adequate protection from Covid infection and complications. Utmost caution should be applied before embarking on any public policy suggesting/mandating mass-COVID-immunization of healthy children.
Self-reported and physiological reactions to the third BNT162b2 mRNA COVID-19 (booster) vaccine dose
Objective: Evaluate the short-term, self-reported and physiological reactions to the third BNT162b2 mRNA COVID-19 (booster) vaccine dose. Participants: A group of 1,609 (18+ years of age) recipients of at least one dose of the BNT162b2 vaccine. 1,344 of the participants were recipients of the third vaccine dose. Results: The extent of systemic reactions reported following the third (booster) dose administration is similar to that reported following the second dose (p-value=0.305) and considerably greater than that reported following the first dose (p-value<0.001). Our analyses of self-reported well-being indicators as well as the objective heart rate and heart rate variability measures recorded by the smartwatches further support this finding. Focusing on the third dose, reactions were more apparent in younger participants (p-value<0.01), in women (p-value<0.001), and in participants with no underlying medical conditions (p-value<0.001). Nevertheless, reported reactions and changes in physiological measures returned to their baseline levels within three days from inoculation with the third dose. Our work further supports the safety of a third COVID-19 BNT162b2 mRNA (booster) vaccine dose.
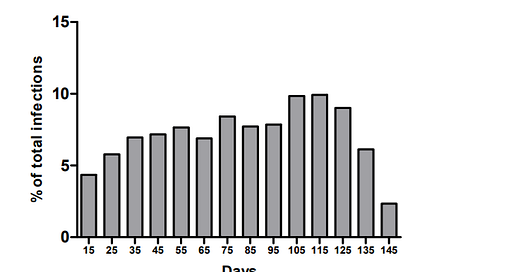
Effectiveness of COVID-19 Vaccines: Eight Months Post Single Dose Vaccination
A total of 18,543 subjects received a single-dose of either of the vaccines at one vaccination centre in the Kingdom of Saudi Arabia (KSA). 92.17% of the subjects had no COVID-19 infection post-vaccination. Diabetes mellitus (p=0.0325), organ transplantation (p=0.0254), and morbid obesity (p=0.0014) were risk factors for infection post-vaccination. Unlike vaccine type, being Saudi, male, or obese was more likely to get the infection earlier. Single-dose COVID-19 vaccines in KSA showed an effectiveness rate of 92.17% up to eight months follow-up. The rate for AZD1222 was higher than what have been previously reported.